Factors Associated with Self - care behaviors of Patients with Chronic Schizophrenia
Keywords:
Self-care behaviors, Social support, Self-efficacy, Family function, Patients with chronic schizophreniaAbstract
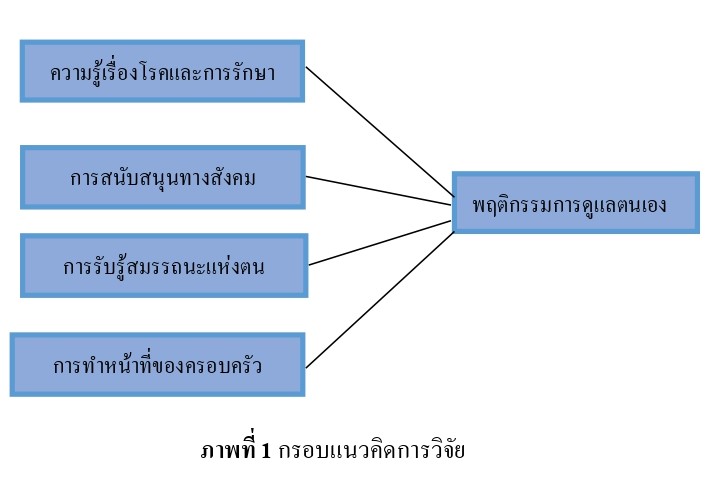
The descriptive study aimed to determine relationship among knowledge of the disease and drug-assisted treatment, social support, self-efficacy, and family function in relation to self-care behaviors of 90 patients with chronic schizophrenia who were treated with medication or monitored at a psychiatric clinic in Kalasin province using a purposive sample technique. The questionnaires used to collect the data were: 1) Personal information questionnaire; 2) Self-care behavior assessment; 3) Knowledge of the disease and drug-assisted treatment measurement; 4) Social support measurement; 5) Self-efficacy measurement; and 6) Family function measurement. The reliability indexes for parts 2, 3, 4, 5, and 6 were 0.87, 0.92, 0.80, 0.80, and 0.88, respectively. The data were analyzed by using descriptive statistics and Pearson correlation analysis.
According to the results, the majority of patients with chronic schizophrenia were male, and they exhibited good self-care behaviors (x ̅ = 132.73, S.D. = 6.47). Knowledge of the disease and drug-assisted treatment, social support, and self-efficacy, all had statistically significant moderately positive relationships with self-care behaviors at the 0.5 level (r =.497, p =.000; r =.498, p =.000; r =.573, p =.000, respectively). However, there was no statistically significant negative association between self-care behaviors and family function (r = -.028, p =.795).
The study's findings may serve as baseline information to enhance recommendations for encouraging self-care behaviors.
References
Awarulhak, T. (2019). Perceived Factors and Social Support of Caregivers of the Schizophrenics in Relation to Medication Behavior of the Schizophrenics in Waeng District Narathiwat Province. Journal of Department of Health Service Support, 15(2), 42 - 50. https://thaidj.org/ index.php/jdhss/article/view/7982.
Behera, S., Bhowmick, I., & Kumar, P. (2024). Family functioning in persons with schizophrenia: Cross sectional study across the genders. Indian Journal of Psychiatric Social Work, 15(2), 3 - 10. https://www.pswjournal.org/index.php/ijpsw/article/view/616
Calatrava, M., Martins, M. V., Schweer-Collins, M., Duch-Ceballos, C., & Rodríguez-González, M. (2022). Differentiation of self: A scoping review of Bowen Family Systems Theory’s core construct. Clinical psychology review, 91, 102101. https://doi.org/10.1016/j.cpr.2021.102101
Chen, C., Chen, Y., Huang, Q., Yan, S., & Zhu, J. (2022). Self-care ability of patients with severe Mental disorders: based on community patients’ investigation in Beijing, China. Frontiers in public health, 10, 1 - 9. https://doi.org/10.3389/fpubh.2022.847098.
Chumroonsawas, S. (1993). Effect of Relationship Establishing, Health Teaching and Contracting on Compliance of Schizophrenic Patient in Chiangmai Neuro-Psychiatric Hospital. [Master’s thesis]. Chiangmai University.
Deegan, P. E. (2020). The journey to use medication optimally to support recovery. Psychiatric Services, 71(4), 401 - 402. https://doi.org/10.1176/appi.ps.201900506
Department of Mental Health. (2022, February 8). Mental Health Data Center. https://dmh.go.th/ report/datacenter/hdc/
El Abdellati, K., De Picker, L., & Morrens, M. (2020). Antipsychotic treatment failure: a systematic review on risk factors and interventions for treatment adherence in psychosis. Frontiers in neuroscience, 14, 531763. http://doi.org/10.3389/fnins.2020.531763. eCollection 2020.
Fiorillo, A., Barlati, S., Bellomo, A., Corrivetti, G., Nicolò, G., Sampogna, G., Stanga, V., Veltro, F., Maina, G., & Vita, A. (2020). The role of shared decision-making in improving adherence to pharmacological treatments in patients with schizophrenia: a clinical review. Annals of General Psychiatry, 19, 1 - 12. https://doi:10.1186/s12991-020-00293-4
Hill, L., & Smith, N. (1990). Self-Care Nursing Promotion of Health. Prentice Hall.
Jaftoran, E. A., Keliat, B. A., & Wardani, I. Y. (2021). Nursing intervention, family's role, cadre's role and medical services: Case series on client with hallucination and self-care deficit. Enfermeria Clinica, 31, S180 - S184. https://doi.org/10.1016/j.enfcli.2020.12.018
Jansook, C., Jansook, N., & Railoy, A., (2019). The Effects of Brief Intervention on Medication Adherence Behaviors of Schizophrenic Patients. Journal of The Royal Thai Army Nurses, 20(2), 170 - 177. https://he01.tci-thaijo.org/index.php/JRTAN/article/view/210396/145624
Jiratchayaporn, K., Christraksa, W., & Worrasirinara, P. (2022). The correlation between self-care behavior with application of eastern wisdom and resilience among village health volunteers: a cross-sectional study in southern Thailand. Journal of Population and Social studies, 30, 239 - 250. http://doi.org/10.25133/JPSSv302022.015
Kanthasaibour, P. (2001). An Analysis of Variables Discriminating the Groups of Relapse and Non-relapse Schizophrenic Patients. [Master’s thesis]. Chulalongkorn University.
Karimirad, M. R., Seyedfatemi, N., Mirsepassi, Z., Noughani, F., & Cheraghi, M. A. (2022). Barriers to self-care planning for family caregivers of patients with severe mental illness. Journal of Patient Experience, 9. https://doi.org/10.1177/23743735221092630
Kerdsang, U., Intarakamhang, U., Peungposop, N., & Kerdsang, T. (2022). Health Beliefs, Participation Behavior and Community Rehabilitation Guidelines Forschizophrenia Patients. The Journal of Psychiatric Nursing and Mental Health, 36 (2), 1 - 21. https://he02.tci-thaijo.org/index. php/JPNMH/article/view/255235/176680
Lani, T., & Sitanggang, Y. A. (2024). Family Support in Fulfilling Activities of Daily Living and the Level of Personal Hygiene-Bathing in Schizophrenia Patients. Jurnal Keperawatan Komprehensif (Comprehensive Nursing Journal), 10(1). 19 – 23 https://doi.org/10.33755 /jkk.v10i1.647
Lee, H. Y., Hwang, J., Ball, J. G., Lee, J., Yu, Y., & Albright, D. L. (2020). Mental health literacy affects mental health attitude: Is there a gender difference. American Journal of Health Behavior, 44(3), 282 - 291. https://doi.org/10.5993/AJHB.44.3.1
Liao, S. J., & Wang, L. J. (2024). Correlation of health literacy, health management self‐efficacy, and attitude in elderly patients with schizophrenia: A cross‐sectional study. Nursing Open, 11(1), e2065. https://doi.org/10.1002/nop2.2065
Liu, D., Zhou, Y., Li, G., & He, Y. (2020). The factors associated with depression in schizophrenia patients: the role of self-efficacy, self-esteem, hope and resilience. Psychology, health & medicine, 25(4), 457 - 469. https://doi.org/10.1080/13548506.2019.1695862
Lotfabadi, M. K., Bayazi, M. H., & Rajaei, A. R. (2022). The effect of cognitive-behavioral group training of self-care skills on self-care in patients with schizophrenia. Nursing Practice Today, 9(1), 24 - 36. https://doi.org/10.18502/npt.v9i1.7327
Ministry of Public Health. (2024, November 22). Health Data Center (HDC). https://hdcservice.moph.go.th/hdc/reports/report.php
Nakharo, J., Kongsuwan, V., & Nukeaw, O. (2023). Factors Predicting Self-Care Behaviors among Prisoners with Schizophrenia. The Southern College Network Journal of Nursing and Public Health, 10(3). e258203. https://he01.tcithaijo.org/index.php/scnet/article/view/258203/179688
Orrico-Sánchez, A., López-Lacort, M., Muñoz-Quiles, C., Sanfélix-Gimeno, G., & Díez-Domingo, J. (2020). Epidemiology of schizophrenia and its management over 8-years period using real-world data in Spain. BMC psychiatry, 20, 19. https://link.springer.com/article/ 10.1186/ s12888-020-02538-8
Ounlam, T. (2020). Nurses’ roles in promoting family functioning of schizophrenia persons in a community. The Journal of Psychiatric Nursing and Mental Health, 34(1),1 - 12. https:// he02.tci-thaijo.org/index.php/jpnmh/article/view/241984?utm.
Pitanupong, J., Ratanaapiromyakij, P., & Teetharatkul, T. (2021). Factors Associated with Low Relapse Rates of Schizophrenia in Southern Thailand: A University Hospital-Based Study. Research Square, 1 - 21. https://doi.org/10.21203/rs.3.rs-922573/v1
Pornsomboon, N. (2017). The effect of Promoting Self-Efficacy Program on Perceived Self-Stigma of persons with Schizophrenia in community. [Master’s thesis]. Chulalongkorn University.
Pothimas, N., Tungpunkom, P., Kanungpiarn, T., & Hannes, K. (2020). Experiences of medication adherence among people with schizophrenia: a qualitative systematic review. Pacific Rim International Journal of Nursing Research, 25(2), 229 - 241. https://he02.tci-thaijo.org/ index.php/PRIJNR/article/view/241815
Sroyphet, J., & Limsaku, M. (2023). A study of social capital that supports families in caring for schizophrenic patients to live in the community: a case study of a community in Bangkok. Journal of MCU Social Development, 8(2), 99 - 112. https://so06.tci-thaijo.org/index.php /JMSD/article/view/264696
Taalab, A. A., Qasem, E. K., Gamal, A. M., & Ashour, E. S. (2021). Dependent Care: Applying Orem Self-Care Theory. Menoufia Nursing Journal, 6(2), 155 - 170. http://doi.org/10.21608/ menj.2021.225860
Thato, R. (2022). Nursing Research: Concepts to Application (6th ed.). Printing House.
Thongkam, A. (2003). Family Functions as Perceived by Persons with Relapsed Schizophrenia. [Independent Study Examining Committee]. Chiangmai University.
Trangkasombut, U., (2018). Family therapy and family counseling (7th ed.). Department of Psychiatry, Faculty of Medicine, Chulalongkorn University.
Tungmephon, P. (2005). Social support, caregiving preparedness and stress among mothers of autistic Children. [Master’s thesis]. Chiangmai University.
Witthawatsamrankun, P. (2021). Quality of Life Among Caregivers of Patients With Schizophrenia at Phrachomklao Hospital Phetchaburi. Region 4 - 5 Medical Journal, 40(1), 19 - 29. https://he02.tcithaijo.org/index.php/reg45/article/view/250060/169919
World Health Organization. (2022, January 10). Schizophrenia. https://www.who.int/news-room/fact-sheets/detail/schizophrenia
Zhang, T., Zhao, Z., Wang, X., Yang, B., Li, M., Wang, L., Yang, C., Fu, C., Li, Z., Zhang, X., Guo, Y., Zhang, N., Pu, E., & Yin, J. (2024).
Sequential mediation model of social support, care burden, and internalized stigma among family function and depression in caregivers of patients with schizophrenia: evidence from a cross-sectional study in southwest China. Social Psychiatry and Psychiatric Epidemiology, 1 - 13. https://link.springer.com/article/10.1007/ s00127-024-02753-8
Zhang, X., Liu, L., Ning, J., Wu, S., Li, S., Zhang, Z., & Li, X. (2022). Factors Influencing Self-Management of Schizophrenia: A Cross-Sectional Study. Journal of Psychosocial Nursing and Mental Health Services, 61(2),19 – 26. https://doi.org/10.3928/02793695-20221027-06.
Zhou, C., & Li, Z. (2020). Modelling of self‐management in schizophrenia: The role of neurocognition, self‐efficacy and motivation. Journal of Clinical Nursing, 29(21-22), 3966 - 3976. https://doi.org/10.1111/jocn.15407
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Princess of Naradhiwas University Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.



