Incidence and Predicting Factors Associated with Complications in Patients with Stroke in Rehabilitation Phase at Thung Khoa Luang Hospital in Roi-Et Province
Keywords:
Incidence, Complications, Patients with stroke, Rehabilitation phaseAbstract
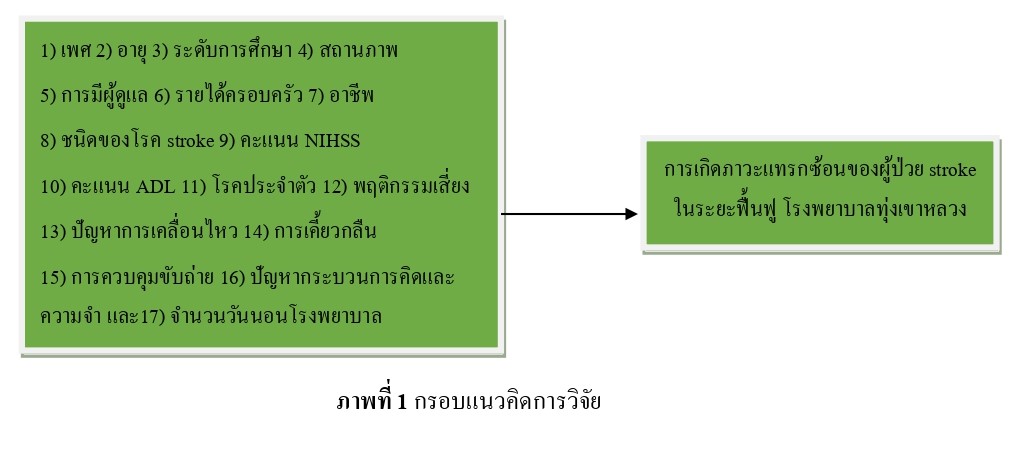
This descriptive retrospective analysis research aimed to study incidence and predicting factors associated with complications in patients with stroke in rehabilitation phase at Thung Khoa Luang Hospital in Roi-Et Province. Samples were 136 patients with stroke in rehabilitation phase who were admitted in inpatient ward at Thung Khoa Luang Hospital between January 1, 2018, and December 31, 2022, and who met the inclusion criteria. Data were collected from medical records by using a data record form with a content validity of 1. Sample data were analyzed by using descriptive statistics and multiple logistic regression statistics.
The findings showed that from 136 samples had complications (58.09%), which were divided among pneumonia (44.30%), pressure sores (32.91%), urinary tract infections (13.92%), and joint stiffness and muscular atrophy (8.86%). Predicting factors associated with complications in patients with stroke in rehabilitation phase at Thung Khoa Luang Hospital were male (OR Adj 3.56; 95 %
CI = 1.33, 9.54; p = 0.012), those with Activity Daily Living scores between 25 and 45 (OR Adj 7.38; 95% CI = 1.48, 36.89; p = 0.015), those with Activity Daily Living score between 75 and 90 (OR Adj 4.64; 95 % CI = 1.08, 19.86; p = 0.039), dysphagia issues (OR Adj 9.06; 95 % CI = 2.66, 30.85; p < 0.001), and urine and bowel incontinence (OR Adj 9.35; 95 % CI = 1.41, 61.86; p = 0.020).
References
Ahmad, M., Ayaz, Z., Sinha, T., Soe, T. M., Tutwala, N., Alrahahleh, A. A., Arrey Agbor, D. B., & Ali, N. (2024). Risk Factors for the Development of Pneumonia in Stroke Patients: A Systematic Review and Meta-Analysis. Cureus, 16(3), e57077. https://doi.org/10.7759 /cureus.57077
Badve, M.S., Zhou, Z., van de Beek, D., Anderson, C.S., & Hackett, M.L. (2019). Frequency of post-stroke pneumonia: Systematic review and meta-analysis of observational studies. International journal of stroke: official journal of the International Stroke Society, 14(2), 125 – 136. https://doi.org/10.1177/1747493018806196
Balcerak, P., Corbiere, S., Zubal, R., & Kägi, G. (2022). Post-stroke Dysphagia: Prognosis and Treatment-A Systematic Review of RCT on Interventional Treatments for Dysphagia Following Subacute Stroke. Frontiers in neurology, 13, 823189. https://doi.org/10.3389/ fneur.2022.823189
Chohan, S.A., Venkatesh, P.K., & How, C.H. (2019). Long-term complications of stroke and secondary prevention: an overview for primary care physicians. Singapore medical journal, 60(12), 616 – 620. https://doi.org/10.11622/smedj.2019158
Cicek, E.D., Alkan, A.Ö., Yukselen, N.P., Onal, Y., Karakas, H.M., & Vural, A. (2024). Pressure ulcer development in patients treated for acute ischaemic stroke. Journal of wound care, 33(6), 441 – 449. https://doi.org/10.12968/jowc.2020.0331
Elkind, M.S., Boehme, A.K., Smith, C.J., Meisel, A., & Buckwalter, M.S. (2020). Infection as a Stroke Risk Factor and Determinant of Outcome After Stroke. Stroke, 51(10), 3156 – 3168. https://doi.org/10.1161/STROKEAHA.120.030429
Garavelli, F., Ghelfi, A.M., & Kilstein, J. G. (2021). Usefulness of NIHSS score as a predictor of non-neurological in-hospital complications in stroke. Utilidad del score NIHSS como predictor de complicaciones intrahospitalarias no neurológicas en ictus isquémico. Medicina clinica, 157(9), 434 – 437. https://doi.org/10.1016/j.medcli.2020.07.034
Gu, M., & Huang, H. (2023). Effect of early rehabilitation nursing on neurological function and quality of life of patients with hemiplegia after stroke: A meta-analysis. Medicine, 102(34), e34919. https://doi.org/10.1097/MD.0000000000034919
Health Administration division Office of Permanent Secretary. (2019). Guideline for intermediate care. Born to be publishing.
Hosmer, D.W., & Lemeshow, S. (2000) Applied logistic regression (2nd Ed.). John Wiley & Sons.
Jullamate, P. (2021). Geriatric nursing, Cerebrovascular disease [Master’s thesis]. Burapha University.
Leangpanich, N., Chuphanitsakun, Y., Pakaranodom, K., Kerdjarern, K., & Poonual, W. (2019). Scoring Of Post Stroke Pneumonia In Uttaradit Hospital. Journal of multidisciplinary healthcare, 12, 917 – 923. https://doi.org/10.2147/JMDH.S218654
Neurological Institute of Thailand. (2015). Clinical Nursing Practice Guideline for Stroke. Tana Press Co., Ltd.
Pairohsathien, S. (2023). Association between the Severity of Acute Ischemic Stroke and its Complications after Hospitalization. Singburi Hospital Journal. 23(1), B1 - B13. https://he01.tci-thaijo.org/index.php/shj/article/view/262661
Pukkaeraka, W., Somgit, W., Vibulchai, N., & Dejsiri, S. (2022). Development of a Nursing Management Model for Preventing Pressure Ulcers among Neurosurgical Critical Patients. Journal of Phrapokklao Nursing College, Chanthaburi, 33(2), 81 – 98. https://he01.tci-thaijo.org/index.php/pnc/article/view/259146
Schwarzbach, C.J., & Grau, A.J. (2020). Komplikationen nach Schlaganfall: Klinische Herausforderungen in der Schlaganfallnachsorge [Complications after stroke: Clinical challenges in stroke aftercare]. Der Nervenarzt, 91(10), 920 – 925. https://doi.org/10.1007/ s00115-020-00988-9
Somgit, W., Srisawas P., & Phuthikhamin N. (2021). Factors Predicting Pneumonia in Stroke Patients: A Systematic Review. Royal Thai Navy Medical Journal. 48(3), 742 – 758. https://he01.tci-thaijo.org/index.php/nmdjournal/article/view/253412
Tater, P., & Pandey, S. (2021). Post-stroke Movement Disorders: Clinical Spectrum, Pathogenesis, and Management. Neurology India, 69(2), 272 – 283. https://doi.org/10.4103/0028-3886. 314574
Tiamkao, S. (2022). Stroke: Situation report. Thai Journal of Neurology. 39(2), 39 – 46.
http://neurothai.org/images/journal/2023/vol39_no2/06%20Original%20Somsak%20Ubatkarn.pdf
Thung Khoa Luang Hospital. (2023). Statistics report: incidence report. Author.
Wang, S., Zou, X.L., Wu, L.X., Zhou, H.F., Xiao, L., Yao, T., Zhang, Y., Ma, J., Zeng, Y., & Zhang, L. (2022). Epidemiology of intracerebral hemorrhage: A systematic review and meta-analysis. Frontiers in neurology, 13, 915813. http://doi.org/10.3389/fneur.2022.915813
World Stroke Organization. (2022, August 3). ANNUAL REPORT 2022. https://www.world-stroke.org/assets/downloads/WSO_Annual_Report_2022_-_online.pdf
Xu, C.Y., Ye, H.W., Chen, B., Wu, Y.F., Cao, Z., Ding, Z., Yao, Y.P., Gao, Y., Li, J., Zhu, J. J., & He, S. (2021). Analysis of risk factors and prognosis of post-stroke pulmonary infection in integrated ICU. European review for medical and pharmacological sciences, 25(2), 856 – 865. https://doi.org/10.26355/eurrev_202101_24654
Yoshimura, Y., Wakabayashi, H., Bise, T., Nagano, F., Shimazu, S., Shiraishi, A., Yamaga, M., & Koga, H. (2018). Sarcopenia is associated with worse recovery of physical function and dysphagia and a lower rate of home discharge in Japanese hospitalized adults undergoing convalescent rehabilitation. Nutrition (Burbank, Los Angeles County, Calif.), 61, 111 – 118. https://doi.org/10.1016/j.nut.2018.11.005
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Princess of Naradhiwas University Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.



