Prevalence and factors associated with acute exacerbation among chronic obstructive pulmonary disease patients in a community hospital
Keywords:
Chronic obstructive pulmonary disease, Acute exacerbation, Prevalence, Community hospitalsAbstract
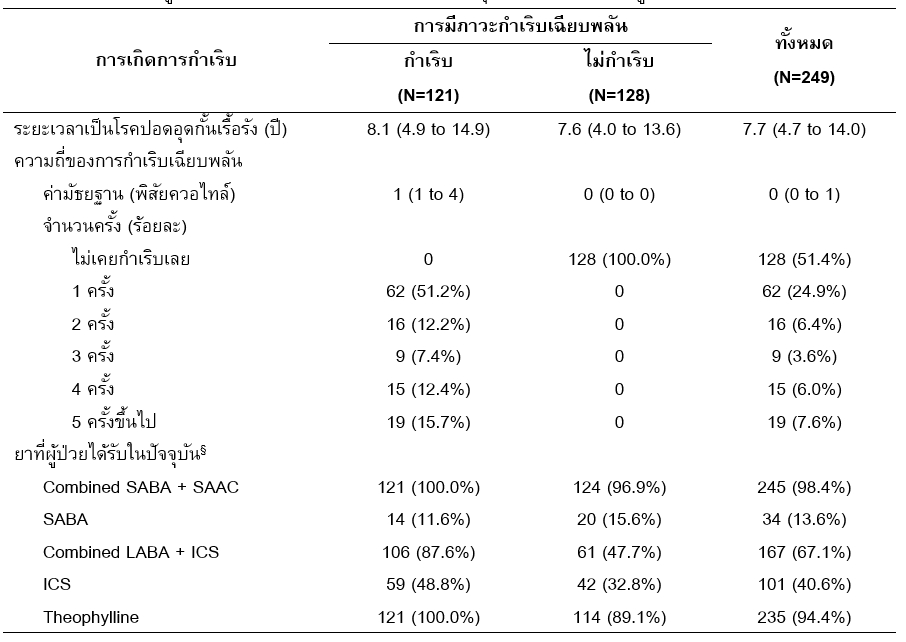
This study aims to examine the prevalence of chronic obstructive pulmonary disease (AECOPD) and its associated factors in COPD patients. We performed a retrospective study in 249 COPD patients who were initially diagnosed and registered at the COPD clinic at Chun hospital, Phayao, by collecting data from medical records during 1st October 2018 and 30th April 2020. Results were further analyzed using uni- and multivariable logistic and negative binomial regression to investigate the association of the following factors: age, blood pressure, body mass index, duration of COPD, smoking status, alcohol drinking status, comorbidities, occupation, and current COPD medications, on the risk of AECOPD and its frequency. The results had shown that the prevalence of AECOPD during the study period was 48.6%. Moreover, a factor associated with increased risk of AECOPD was receiving combined beta2 agonists and corticosteroids (Odds ratio 7.14 [95%CI 1.78 to 28.66]). In comparison, factors associated with the increased frequency of AECOPD were the duration of the disease (Incidence rate ratio per year increase was 0.77 [95%CI 0.71 to 0.83]) and alcohol drinking status (Incidence rate ratio 0.19 [95%CI 0.02 to 0.64]). Although the findings might be a consequence of reverse causality and survival bias, the high prevalence rate and its significant frequency in those with a recent diagnosis may indicate the need for closer monitoring or more intensive treatment in this particular group of patients.
References
Barbara W, Joseph D, Terry S, Cecily D. Pharmacotherapy handbook. 9th ed. New York]: McGraw-Hill Education; 2014.
World Health Organization. Chronic obstructive pulmonary disease (COPD) [Internet]. [cited 2021 Apr 18]. Available from: http://www.emro.who.int/health-topics/chronic-obstructive-pulmonary-disease-copd/index.html
Mathers CDD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
Service Plan COPD. Guideline for the management of chronic obstructive pulmonary disease (COPD). Phayao: Phayao Provincial Public Health Office in collaboration with Phayao Hospital; 2020.
Müllerova H, Maselli DJ, Locantore N, Vestbo J, Hurst JR, Wedzicha JA, et al. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest. 2015;147(4):999–1007.
Roberts M, Mapel D, Von Worley A, Beene J. Clinical factors, including all patient refined diagnosis related group severity, as predictors of early rehospitalization after COPD exacerbation. Drugs Context. 2015;4:1–15.
Global Initative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2021 report [Internet]. 2021 [cited 2021 Aug 10]. Available from: https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf
Guideline for the treatment of chronic obstructive pulmonary disease 2017. Bangkok: Thoracic Society of Thailand Under Royal Patronage; 2017.
Hwang Y Il, Lee SH, Yoo JH, Jung BH, Yoo KH, Na MJ, et al. History of pneumonia is a strong risk factor for chronic obstructive pulmonary disease (COPD) exacerbation in South Korea: the Epidemiologic review and Prospective Observation of COPD and Health in Korea (EPOCH) study. J Thorac Dis. 2015;7(12):2203–13.
Garcia-Aymerich J, Farrero E, Félez MA, Izquierdo J, Marrades RM, Antó JM. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax. 2003;58(2):100–5.
García-Sanz MT, Pol-Balado C, Abellás C, Cánive-Gómez JC, Antón-Sanmartin D, González-Barcala FJ. Factors associated with hospital admission in patients reaching the emergency department with COPD exacerbation. Multidiscip Respir Med. 2012;7(1):6.
Alexopoulos EC, Malli F, Mitsiki E, Bania EG, Varounis C, Gourgoulianis KI. Frequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study). Int J Chron Obstruct Pulmon Dis. 2015;10:2665–74.
Pothirat C, Pothirat T, Liwsrisakun C, Bumroongkit C, Deesomchok A, Theerakittikul T, et al. Risk factors of severe acute exacerbation of chronic obstructive pulmonary disease among patients regularly managed by pulmonologists. J Med Assoc Thai. 2017;100(2):142–8.
Vatcheva KP, Lee M, McCormic JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology. 2016;6(2):1–9.
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393.
Carpenter J, Kenward M. Multiple imputation and its application. Chichester, United Kingdom: John Wiley & Sons; 2013.
Calverley PMA, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–89.
Palanupap K, Wacharamaneekan K, Khameiad T, Treetrisit P, Kantasa P, Chowjiriyapan K, et al. Risk factors associated 28-day readmission for a chronic obstructive pulmonary disease exacerbation. Naresuan Phayao Journal. 2016;9(2):13–6.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Muraki M, Kunita Y, Shirahase K, Yamazaki R, Hanada S, Sawaguchi H, et al. A randomized controlled trial of long-acting muscarinic antagonist and long-acting β2 agonist fixed-dose combinations in patients with chronic obstructive pulmonary disease. BMC Pulm Med. 2021;21(1):1–8.
Calverley PMA, Anzueto AR, Carter K, Grönke L, Hallmann C, Jenkins C, et al. Tiotropium and olodaterol in the prevention of chronic obstructive pulmonary disease exacerbations (DYNAGITO): a double-blind, randomised, parallel-group, active-controlled trial. Lancet Respir Med. 2018;6(5):337–44.
Buhl R, Maltais F, Abrahams R, Bjermer L, Derom E, Ferguson G, et al. Tiotropium and olodaterol fixed-dose combination versus mono-components in COPD (GOLD 2-4). Eur Respir J. 2015;45(4):969–79.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Naresuan Phayao Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผู้นิพนธ์ต้องรับผิดชอบข้อความในบทนิพนธ์ของตน มหาวิทยาลัยพะเยาไม่จำเป็นต้องเห็นด้วยกับบทความที่ตีพิมพ์เสมอไป ผู้สนใจสามารถคัดลอก และนำไปใช้ได้ แต่จะต้องขออนุมัติเจ้าของ และได้รับการอนุมัติเป็นลายลักษณ์อักษรก่อน พร้อมกับมีการอ้างอิงและกล่าวคำขอบคุณให้ถูกต้องด้วย
The authors are themselves responsible for their contents. Signed articles may not always reflect the opinion of University of Phayao. The articles can be reproduced and reprinted, provided that permission is given by the authors and acknowledgement must be given.