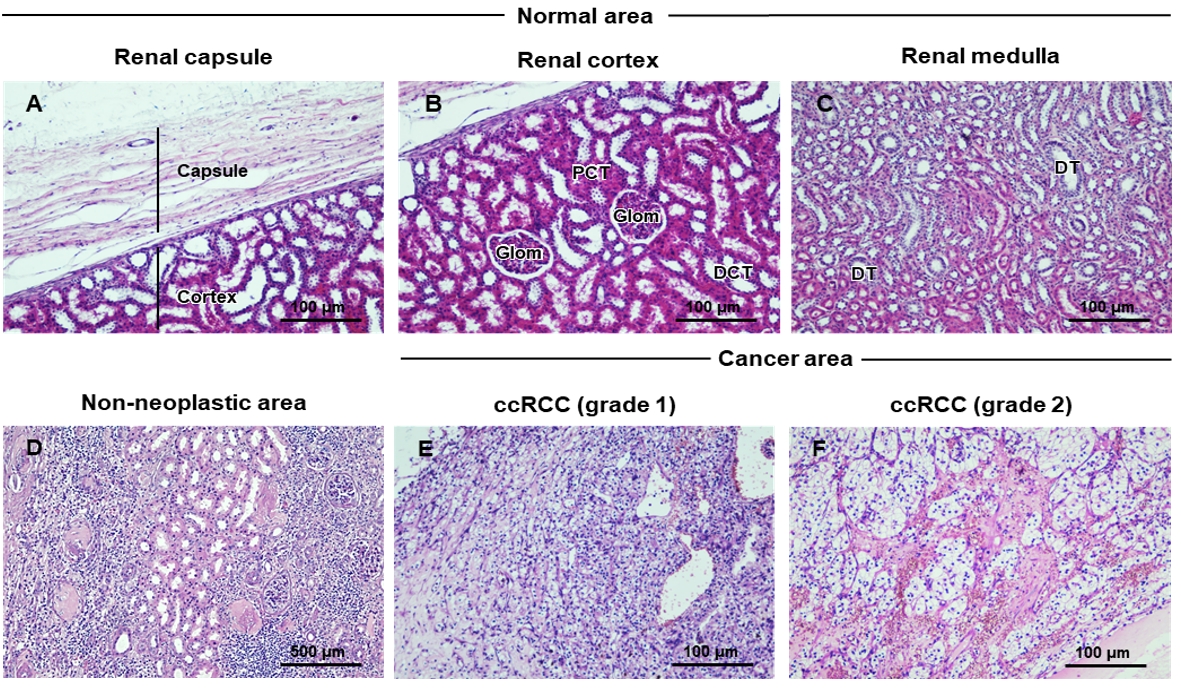
Histopathological features of non-neoplastic areas of clear cell renal cell carcinoma tissues and clinical outcomes of patients
Keywords:
Clear cell, Histopathologic features, Non-neoplastic area, Renal cell carcinomaAbstract
This study aimed to investigate the histopathological changes in non-neoplastic areas of clear cell renal cell carcinoma tissue, using H&E and PAS staining, and to evaluate the clinical outcomes of patients. Our findings illustrated several aspects of the histopathological features of non-neoplastic areas of renal cancer tissues. It consisted of mononuclear infiltration, adipocyte deposition, interstitial fibrosis with macrophage infiltration, and fibrinoid necrosis of the interlobar arteries. Nodular glomerulosclerosis along with thickening of glomerular basement membranes was abundant in the non-neoplastic area. The hemorrhagic area was remarkable for containing RBC casts and macrophages containing hemosiderin. Additionally, we found necrosis of the renal tubular epithelium, thyroidization, and inflammatory cells casts in the tubular lumen. Most of our patients were elderly and the neoplasms presented mostly in males. The specimens were mostly found to show chronic pyelonephritis (64.71%) and hemorrhagic areas (88.24%). The patients were observed to have metastatic status (17.65%) and had been diagnosed with chronic pyelonephritis. All 8/17 patients had a comorbidity e g. hypertension (HT), chronic kidney disease (CKD), diabetes mellitus (DM). We noted that ccRCC patients presenting with chronic pyelonephritis and with metastases had cumulative survival rates lower than those patients without chronic pyelonephritis (72% vs. 100%). Hence, evaluation of histopathological changes in non-neoplastic renal parenchyma should be performed for patients with RCC, to improve management and treatment options, that may prevent accelerated function failure of the single remaining kidney, especially in patients with a background of medical diseases, including diabetes or hypertension.
References
Padala SA, Barsouk A, Thandra KC, Saginala K, Mohammed A, Vakiti A, et al. Epidemiology of Renal Cell Carcinoma. World J Oncol 2020;11(3):79-87.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA: Cancer J Clin 2020;70(1):7-30.
Rini BI, Campbell SC, Escudier B. Renal cell carcinoma. Lancet 2009;373(9669):1119-32.
Capitanio U, Montorsi F. Renal cancer. Lancet 2016;387(10021):894-906.
Ellis RJ. Chronic kidney disease after nephrectomy: a clinically-significant entity? Transl Androl Urol 2019;8(Suppl 2):S166-S74.
Bijol V, Mendez GP, Hurwitz S, Rennke HG, Nosé V. Evaluation of the nonneoplastic pathology in tumor nephrectomy specimens: predicting the risk of progressive renal failure. Am J Surg Pathol 2006;30(5):575-84.
Noroozinia F, Makhdoomi K, Behnamfard H, Mohammadi S, Dindarian S, Bagheri M, et al. The pathological evaluation of nonneoplastic kidney disorder in tumor nephrectomy specimens. Saudi J Kidney Dis Transpl 2018;29(3):586-90.
Henriksen KJ, Meehan SM, Chang A. Non-neoplastic renal diseases are often unrecognized in adult tumor nephrectomy specimens: a review of 246 cases. Am J Surg Pathol 2007;31(11):1703-8.
Bonsib SM, Pei Y. The Non-neoplastic Kidney in Tumor Nephrectomy Specimens: What Can it Show and What is Important? Adv Anat Pathol 2010;17(4):235-50.
Corti B, Zucchini N, Fabbrizio B, Martorana G, Schiavina R, Grigioni ADE, et al. Pathology and Molecular Pathogenesis of Renal Cell Carcinoma. Eur Urol Suppl 2006;5(8):573-9.
Fuhrman SA, Lasky LC, Limas C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 1982;6(7):655-63.
Petejova N, Martinek A. Renal cell carcinoma: Review of etiology, pathophysiology and risk factors. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc Czech Repub 2016;160(2):183-94.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th Edition of the AJCC Cancer Staging Manual and the Future of TNM. Ann Surg Oncol 2010;17(6):1471-4.
Chow W-H, Dong LM, Devesa SS. Epidemiology and risk factors for kidney cancer. Nat Rev Urol 2010;7(5):245-57.
Streja E, Kalantar-Zadeh K, Molnar MZ, Landman J, Arah OA, Kovesdy CP. Radical versus partial nephrectomy, chronic kidney disease progression and mortality in US veterans. Nephrol Dial Transplant 2016;33(1):95-101.
Bijol V, Batal I. Non-neoplastic Pathology in Tumor Nephrectomy Specimens. Surg Pathol Clin 2014;7(3):291-305.
Salvatore SP, Cha EK, Rosoff JS, Seshan SV. Nonneoplastic renal cortical scarring at tumor nephrectomy predicts decline in kidney function. Arch Pathol Lab Med 2013;137(4):531-40.
Garcia-Roig M, Gorin MA, Parra-Herran C, Garcia-Buitrago M, Kava BR, Jorda M, et al. Pathologic evaluation of non-neoplastic renal parenchyma in partial nephrectomy specimens. World J Urol 2013;31(4):835-9.
Truong LD, Shen SS, Park MH, Krishnan B. Diagnosing nonneoplastic lesions in nephrectomy specimens. Arch Pathol Lab Med 2009;133(2):189-200.
Higgins JP, McKenney JK, Brooks JD, Argani P, Epstein JI. Recommendations for the reporting of surgically resected specimens of renal cell carcinoma: the Association of Directors of Anatomic and Surgical Pathology. Hum Pathol 2009;40(4):456-63.
Gautam G, Lifshitz D, Shikanov S, Moore JM, Eggener SE, Shalhav AL, et al. Histopathological predictors of renal function decrease after laparoscopic radical nephrectomy. J Urol 2010;184(5):1872-6.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Naresuan Phayao Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผู้นิพนธ์ต้องรับผิดชอบข้อความในบทนิพนธ์ของตน มหาวิทยาลัยพะเยาไม่จำเป็นต้องเห็นด้วยกับบทความที่ตีพิมพ์เสมอไป ผู้สนใจสามารถคัดลอก และนำไปใช้ได้ แต่จะต้องขออนุมัติเจ้าของ และได้รับการอนุมัติเป็นลายลักษณ์อักษรก่อน พร้อมกับมีการอ้างอิงและกล่าวคำขอบคุณให้ถูกต้องด้วย
The authors are themselves responsible for their contents. Signed articles may not always reflect the opinion of University of Phayao. The articles can be reproduced and reprinted, provided that permission is given by the authors and acknowledgement must be given.