Factors Affecting the Blood Level of Phenytoin in Thai Children with Epilepsy: A retrospective study
Pawalee Niamtaworn
Keywords:
Drug level, Children, Phenytoin, epilepsyAbstract
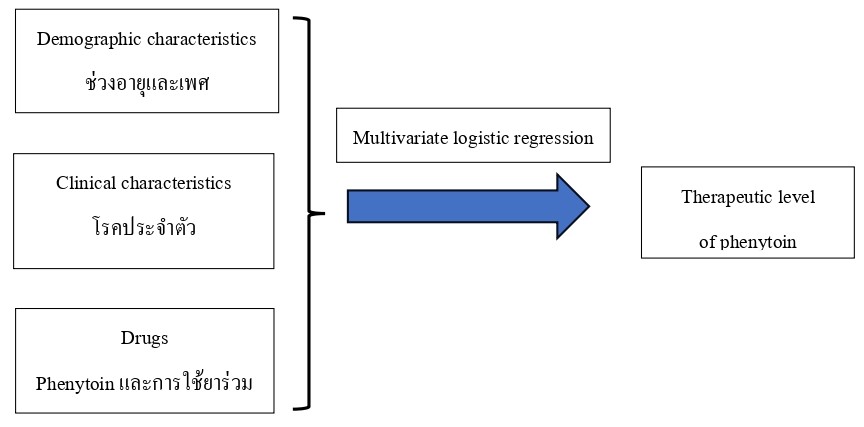
Phenytoin is a medication for epilepsy with a narrow therapeutic index. There is not nearly as much at the therapeutic level in children. Therefore, it is very crucial to study the factors affecting the blood level of phenytoin. This study aimed to study factors affecting the blood level of phenytoin in Thai children with epilepsy, aged 1 month to 18 years, who were hospitalized to tertiary hospitals between 2014 and 2018. The cross-sectional study was used to gather electronic data. Data analysis utilized in this study was Multivariate logistic regression. The results found that phenytoin was administered to 275 subjects. A blood level of phenytoin test was administered 107 times to the 59 subjects. The blood level of phenytoin was statistically substantially correlated with gender, age group, comorbidities, and highly protein bound drugs (p<0.05). Phenytoin levels in the blood were associated with male gender, infant group, comorbidities, and highly protein bound drugs. In contrast to the teenage group, the toddler group had a factor associated with the blood level of phenytoin. In conclusion, age group, comorbidities, and highly protein bound drugs should be taken into consideration when administrating phenytoin. These factors affect the blood level of phenytoin, which can become ineffective in controlling epileptic symptoms and medicine safety.
References
Garofalo, E. (2007). Clinical Development of Antiepileptic Drugs for Children. Neurotherapeutics, 4(1), 70 - 74.
Houghton, G.W., Richens, A., & Leighton, M. (1975). Effect of age, height, weight and sex on serum phenytoin concentration in epileptic patients. British Journal of Clinical Pharmacology, 2(3), 251 - 256. DOI:10.1111/j.1365-2125.1975.tb01583.x
Ismail, R., Rahman, A., & Chand, P. (1994). Pharmacokinetics of phenytoin in routine clinic patients in Malaysia. Journal of clinical pharmacy and therapeutics, 19(4), 245 - 248.
Jun, H., Rong, Y., Yih, C., Ho, J., Cheng, W., & Kiang, T. K. (2020). Comparisons of Four Protein-Binding Models Characterizing the Pharmacokinetics of Unbound Phenytoin in Adult Patients Using Non-Linear Mixed-Effects Modeling. Drugs in R&D, 20(4), 343 - 358.
Karaźniewicz-Łada, M., Główka, A.K., Mikulska, A.A., Główka, F.K., (2021). Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients. International Journal of Molecular Sciences. 22(17), 9582. DOI:10.3390/ijms22179582
Karol, M.D., Locke, C.S., & Cavanaugh, J.H. (1999). Lack of pharmacokinetic interaction between lansoprazole and intravenously administered phenytoin. The Journal of Clinical Pharmacology, 39(12), 1283 - 1289.
Kutt, H. (1975). Interactions of antiepileptic drugs. Epilepsia, 16(2), 393 - 402.
Marano, M., Nicoletti, F., Pro, S., Goffredo, B., Cecchetti, C., Piervincenzi, E., . . . Cocciadiferro, D. (2020). Phenytoin intoxication associated with omeprazole administration in a child with defective CYP2C9. European journal of clinical pharmacology, 76, 731 - 732.
McDaniel, C.E., Jennings, R., Schroeder, A.R., Paciorkowski, N., Hofmann, M., & Leyenaar, J. (2019). Aligning inpatient pediatric research with settings of care: a call to action. Pediatrics, 143(5), e20182648. DOI:10.1542/peds.2018-2648. PMID: 31018987.
Mekloy, L., & Treyaprasert, W. (2022). Population pharmacokinetics of phenytoin in epileptic children and dosage regimens using Monte Carlo simulation. The Thai Journal of Pharmaceutical Sciences, 46(2), 208 - 215.
Methaset, K., Sathirakul, K., Limpisood, S., Kulsirirat, T., Leethochawalit, S., Chulsom, N., . . . Rukthong, P. (2019). Prediction of phenytoin concentration using STELLATM as a pharmacokinetic modeling program. Isan Journal of Pharmaceutical Sciences, 15(2), 44 - 50.
Mir, S.A. (2019). Effect of age and sex on serum phenytoin concentration in epileptic patients: experience from therapeutic drug monitoring. International Journal of Basic & Clinical Pharmacology, 8(8), 1717 – 1721. DOI: 10.18203/2319-2003.ijbcp20193169
Murphy, A., & Wilbur, K. (2003). Phenytoin–Diazepam Interaction. Annals of Pharmacotherapy. 37(5), 659 - 663. DOI:10.1345/aph.1C413
Patsalos, P.N., Spencer, E.P., & Berry, D. J. (2018). Therapeutic Drug Monitoring of Antiepileptic Drugs in Epilepsy: A 2018 Update. Therapeutic Drug Monitoring, 40(5), 526 - 548. DOI:10.1097/ftd.0000000000000546
Paul, H.A., Robinson, J.L., & Sadrzadeh, S.H. (2020). Free versus total phenytoin measurements—a case study of phenytoin toxicity Toxicology Cases for the Clinical and Forensic Laboratory, 131-133, Academic Press.
Rane, A., & Wilson, J.T. (1976). Clinical pharmacokinetics in infants and children. Clinical Pharmacokinetics, 1, 2 - 24. DOI: 10.2165/00003088-197601010-00002. PMID: 1017153.
Srivastava, K., Bhartiya, S., Gavli, V., Patil, R., & Rajadhyaksha, S. (2020). Efficacy, Tolerability and Serum Phenytoin Levels after Intravenous Fosphenytoin Loading Dose in Children with Status Epilepticus. Indian Pediatr, 57(3), 218 - 221.
Stiles-Shields, C., Plevinsky, J. M., Psihogios, A. M., & Holmbeck, G. N. (2020). Considerations and future directions for conducting clinical research with pediatric populations during the COVID-19 pandemic. Journal of Pediatric Psychology, 45(7), 720-724.
Suzuki, Y., Mimaki, T., Cox, S., Koepke, J., & Hayes, J. (1994). Phenytoin Age-Dose-Concentration Relationship in Children. Therapeutic Drug Monitoring, 16(2), 145 - 150.
van Dijkman, S.C., Rauwé, W.M., Danhof, M., & Della Pasqua, O. (2018). Pharmacokinetic interactions and dosing rationale for antiepileptic drugs in adults and children. British Journal of Clinical Pharmacology, 84(1), 97 - 111.
Verrotti, A., Iapadre, G., Di Donato, G., Di Francesco, L., Zagaroli, L., Matricardi, S., . . . Iezzi, M. L. (2019). Pharmacokinetic considerations for anti-epileptic drugs in children. Expert Opinion on Drug Metabolism & Toxicology, 15(3), 199 - 211.DOI:10.1080/17425255.2019.1575361
Wisuttiwong, P. (2007). Pharmacokinetic parameters of phenytoin in Thai epileptic children. Chulalongkorn University. (in Thai).
Wolf, G., McClain, C., Zurakowski, D., Dodson, B., & McManus, M. L. (2006). Total phenytoin concentrations do not accurately predict free phenytoin concentrations in critically ill children. Pediatric Critical Care Medicine, 7(5), 505.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Princess of Naradhiwas University Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.



